Tourette’s Syndrome (TS)
Tourette’s Syndrome (TS) is a neurological condition that causes involuntary movements and sounds, called tics. These can include:
Motor tics – blinking, facial twitches, jerking movements
Vocal tics – coughing, throat clearing, words, or other noises
Tics often change in type, frequency, or intensity. Like autism and ADHD, Tourette’s exists on a spectrum, meaning experiences vary widely from mild to severe, and can even fluctuate day to day.
"Did you know? Swearing (coprolalia) only affects around 10% of people with Tourette’s."


How Tourette’s May Present
(ADHD vs. Tourette Syndrome)

Visible signs:
Sudden repetitive movements
(blinking, head jerks, shoulder shrugs)
Repeating words or sounds
Uncontrollable urges to move or make noises
Tics that worsen with stress, excitement, or tiredness
Premonitory urge (a build-up of tension before a tic)
Hidden struggles:
Pain and chronic fatigue from years of tics
Co-occurring neurodivergence (ADHD, Autism)
Anxiety, depression, OCD, anger, emotional dysregulation
Sleep difficulties
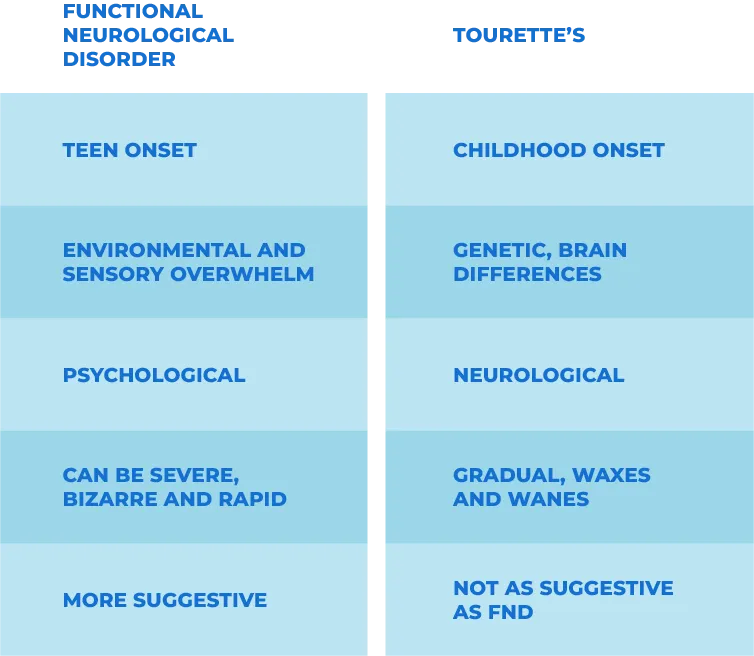
Tourette’s vs. FND (Functional Neurological Disorder)
Tourette’s – neurological, begins in childhood, involuntary, brain-based.
FND – related to nervous system communication, often triggered by trauma, overstimulation, or unmet neurodivergent needs.
Transient vs.
Chronic Tics
Some children experience transient tics, temporary tics that last a few weeks or months, often triggered by stress or developmental changes. These are not Tourette’s, which requires both motor and vocal tics lasting at least one year.
How Tourette Syndrome
Is Diagnosed in the UK
Tourette’s Diagnosis in Children
NHS Pathway
In the UK, children showing signs of tics are usually referred by a GP, teacher, or school nurse to a specialist, often a paediatrician, neurologist, or Child and Adolescent Mental Health Services (CAMHS).
Diagnosis is clinical and based on NICE guidelines, which require:
- At least two motor tics and one vocal tic
- Present for 12 months or more
- Onset before age 18.
The process involves interviews with parents/carers, observation of tics, and ruling out other conditions like autism or ADHD (which often co-occur). No brain scans or blood tests are needed.
Private Assessment for Children
Private routes offer quicker access to specialist assessments. A child neurologist or neurodevelopmental specialist will review the child’s history, observe tics, and use clinical criteria to confirm a diagnosis.
Private providers usually offer full reports for schools and GPs, and may also recommend therapy or behavioural support.
Tourette’s Diagnosis in Adults
NHS Pathway
Adults with tic symptoms usually begin with their GP, who may refer to a neurologist or adult psychiatrist with experience in movement disorders or neurodevelopmental conditions.
Diagnosis is based on:
- Personal and childhood history of tics
- Clinical observation
- Duration and type of tics
Since many adults were undiagnosed as children, assessments may include questions about symptoms going back to early life.
Private Assessment for Adults
Private clinics provide faster assessments with experienced consultants. A detailed history is taken, and diagnostic criteria are applied based on observed and reported symptoms.
Reports often include treatment recommendations such as CBIT (Comprehensive Behavioural Intervention for Tics), medications, or referrals for co-occurring conditions like OCD or ADHD.
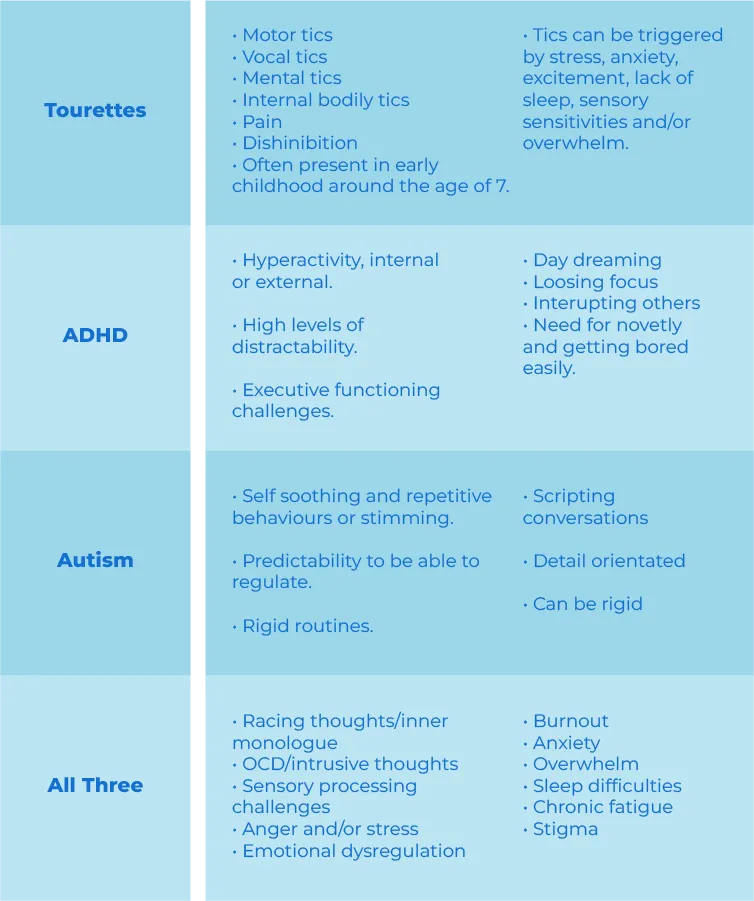
The Tourette’s Trio (Tourette’s, ADHD & Autism)
Some people experience all three conditions together: Tourette’s Syndrome, ADHD, and Autism. Each neurotype influences the others, creating a very individual lived experience.
Autism: can heighten sensory overload, rigid thinking, or difficulties masking tics.
ADHD: adds impulsivity, distractibility, and restless energy, often making tics more frequent or intense.
Tourette’s: may feel harder to manage when combined with the unpredictability of ADHD and the sensory/emotional demands of Autism.
Common Experiences
This neurotype can increase impulsive behaviours, risk-taking, sleep challenges, and emotional ups and downs. It can also complicate attention at school or work, and heighten anxiety from sensory overload or unmet needs.
Finding Balance
While the combination can be challenging, understanding the “Tourette’s Trio” helps families, individuals, and professionals to develop personalised support strategies. Bespoke coaching can explore sensory regulation, routines, and tools that work across all three conditions.
How Support Can Help
With the right strategies, children and adults with Tourette’s can:
✔ Reduce stress triggers that worsen tics.
✔ Learn coping tools for fatigue, pain, and emotional regulation.
✔ Gain confidence in school, work, and social situations.
✔ Build resilience and self-esteem despite challenges.
"Coaching and understanding make a huge difference, not just in managing tics, but in empowering individuals and families to thrive."
Copyright 2024 - 2026. Flourish with Neurodiversity. All Rights Reserved.
Website designed by South Coast Design